what is osteoarthritis?
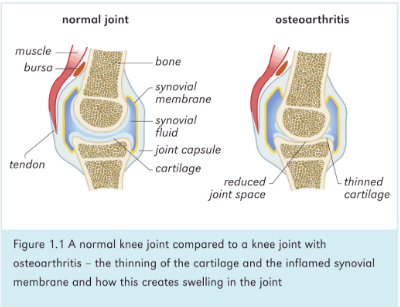
Osteoarthritis is sometimes called 'wear and tear or 'degenerative joint disease'. h is the most common form of arthritis and occurs when the cartilage in your joints becomes thinner over time, or extra bone is laid down around the joint in response to injury or strain. Osteoarthritis can affect any joint in your body, although it most commonly affects joints in your hands, hips. knees and spine.
Typically it affects just one joint, but, as with arthritis of the fingers. several joints can be affected.
Osteoarthritis gradually worsens over time, and no cure exists. It is a natural side-effect of aging. just like gray hair and wrinkles, and in the same way some people will be affected more than others. There are treatments that can relieve pain and help you remain active. By taking steps to exercise you can actively manage your osteoarthritis and gain control over the associated pain.
signs and symptoms
The progression of the bony changes associated with osteoarthritis is slow. The symptoms also develop slowly and worsen over time. The list below outlines the most common symptoms and when you arc most likely to notice them.
• pain in a joint during or after use, or after a period of inactivity
. • swelling - in some cases bur not always.
• tenderness in the joint when you apply light pressure.
• stiffness in and around a joint. which may be most noticeable when you first wake up in the morning or after a period of inactivity.
• loss of flexibility. which may make it difficult to use the joint for normal /functional tasks.
• grating sensation when you move the joint.
• bone spurs, which appear as hard lumps, can form around the affected joint and are seen clearly on X-rays.
Although most commonly felt in the hands, hips, knees and spine, it is possible to develop arthritis in other joints. especially if you have been injured nr placed unusual stress on a joint. It is uncommon for •stecorthritis to affect your jaw, shoulder. elbows, wrists or ankles, but it is possible if you have sustained a fracture or played a span that has increased the stress through a particular joint.
what causes Osteoarthritis Its?
Osteoarthritis occurs when the cartilage covering the ends of bones in your joints becomes thinner over time. The smooth surface of the cartilage becomes rough. causing irritation. Eventually, if the cartilage wears down completely, the surface ends of your bones become worn and your joints become painful. This additional pressure on the bones can make them swell.
In most cases it isn't clear what causes osteoarthritis, but research has shown that it's a combination of thugs. including being overweight. ageing, joint injury or stray. family history and muscle weakness. The most likely causes are:
• Age osteoarthritis typically occurs in older adults. People under 40 rarely experience osteoarthritis.
• Sex: women are more likely to develop osteoarthritis, though it isn't clear why.
• Bone deformities some people are born with joint deformities or defective cartilage, which may increase the risk of osteoarthritis.
• Joint injuries injures that occur whcn playing sports, or from an accident, may increase the risk of developing osteoarthritis.
• Obesity: carrying more body weight places more stress on your weight-bearing joints, such as your knees.
• Other diseases that affect the bones and joints diseases that increase the risk of osteoarthritis include gout, rheumatoid arthritis, Paget's disease of bone and septic arthritis.
12,000 people a year will develop RA. RA affects three times more women than men and onset is generally between 40 and 60 years of age, although you can get the disease at any age. There are around 12,000 children under the age of 16 with the juvenile form of the disease.
We're still not sure what causes RA. Unfortunately there is no cure, but much more is now understood about the inflammatory process associated with the disease and how it can be managed. This book aims to show you how with self-management you can help yourself, and minimize the impact of the disease on your quality of life.
The good news is that if you are diagnosed and treated early, your prognosis is significantly better than it was 20-30 years ago, thanks to research and the development of drugs which can modify the active disease process. Early diagnosis is critical, and research shows that a 3-month window of opportunity exists from onset of symptoms to starting treatment, which can prevent irreversible joint damage. Many people diagnosed now have a good quality of life in spite of having RA, and don't suffer the joint deformity that was once associated with the condition. Research also shows that in reality it can be up to a year between symptoms developing and the start of treatment. It is very important that people know how to recognise the symptoms and see their GP as soon as possible. GP education is also needed to ensure prompt referral for diagnosis and treatment.
Osteoarthritis is sometimes called 'wear and tear or 'degenerative joint disease'. h is the most common form of arthritis and occurs when the cartilage in your joints becomes thinner over time, or extra bone is laid down around the joint in response to injury or strain. Osteoarthritis can affect any joint in your body, although it most commonly affects joints in your hands, hips. knees and spine.
Typically it affects just one joint, but, as with arthritis of the fingers. several joints can be affected.
Osteoarthritis gradually worsens over time, and no cure exists. It is a natural side-effect of aging. just like gray hair and wrinkles, and in the same way some people will be affected more than others. There are treatments that can relieve pain and help you remain active. By taking steps to exercise you can actively manage your osteoarthritis and gain control over the associated pain.
signs and symptoms
The progression of the bony changes associated with osteoarthritis is slow. The symptoms also develop slowly and worsen over time. The list below outlines the most common symptoms and when you arc most likely to notice them.
• pain in a joint during or after use, or after a period of inactivity
. • swelling - in some cases bur not always.
• tenderness in the joint when you apply light pressure.
• stiffness in and around a joint. which may be most noticeable when you first wake up in the morning or after a period of inactivity.
• loss of flexibility. which may make it difficult to use the joint for normal /functional tasks.
• grating sensation when you move the joint.
• bone spurs, which appear as hard lumps, can form around the affected joint and are seen clearly on X-rays.
Although most commonly felt in the hands, hips, knees and spine, it is possible to develop arthritis in other joints. especially if you have been injured nr placed unusual stress on a joint. It is uncommon for •stecorthritis to affect your jaw, shoulder. elbows, wrists or ankles, but it is possible if you have sustained a fracture or played a span that has increased the stress through a particular joint.
what causes Osteoarthritis Its?
Osteoarthritis occurs when the cartilage covering the ends of bones in your joints becomes thinner over time. The smooth surface of the cartilage becomes rough. causing irritation. Eventually, if the cartilage wears down completely, the surface ends of your bones become worn and your joints become painful. This additional pressure on the bones can make them swell.
In most cases it isn't clear what causes osteoarthritis, but research has shown that it's a combination of thugs. including being overweight. ageing, joint injury or stray. family history and muscle weakness. The most likely causes are:
• Age osteoarthritis typically occurs in older adults. People under 40 rarely experience osteoarthritis.
• Sex: women are more likely to develop osteoarthritis, though it isn't clear why.
• Bone deformities some people are born with joint deformities or defective cartilage, which may increase the risk of osteoarthritis.
• Joint injuries injures that occur whcn playing sports, or from an accident, may increase the risk of developing osteoarthritis.
• Obesity: carrying more body weight places more stress on your weight-bearing joints, such as your knees.
• Other diseases that affect the bones and joints diseases that increase the risk of osteoarthritis include gout, rheumatoid arthritis, Paget's disease of bone and septic arthritis.
We're still not sure what causes RA. Unfortunately there is no cure, but much more is now understood about the inflammatory process associated with the disease and how it can be managed. This book aims to show you how with self-management you can help yourself, and minimize the impact of the disease on your quality of life.
The good news is that if you are diagnosed and treated early, your prognosis is significantly better than it was 20-30 years ago, thanks to research and the development of drugs which can modify the active disease process. Early diagnosis is critical, and research shows that a 3-month window of opportunity exists from onset of symptoms to starting treatment, which can prevent irreversible joint damage. Many people diagnosed now have a good quality of life in spite of having RA, and don't suffer the joint deformity that was once associated with the condition. Research also shows that in reality it can be up to a year between symptoms developing and the start of treatment. It is very important that people know how to recognise the symptoms and see their GP as soon as possible. GP education is also needed to ensure prompt referral for diagnosis and treatment.