HOW ARTHRITIS DEVELOPS
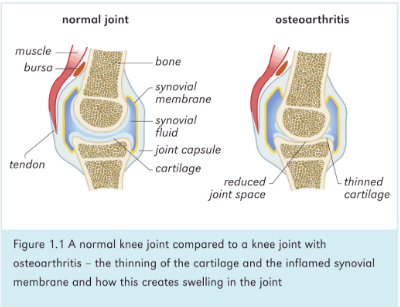
The mechanical construction of our body makes it
possible for many bones to meet with each other and
these meeting places are called joints. These joints help
in different types of movements. To avoid friction and
strain during these movements, the ends of the bone are
covered with an elastic tissue called cartilage. A synovial
membrane covers the inner surfaces of this joint-
cavities. This membrane secretes a fluid that lubricates
the joint.
This synovial membrane and the tips of the bones are
ramified with several capillaries which carry. nourishment
along with blood to the joints. If any infection or wrong
metabolic byproduct passes through these capillaries,
then the circulation of the nutrients and blood is
obstructed resulting in stagnation and exudation of fluid
into the pocket created by the synovial membrane in the
joint. This causes the joints to become inflamed,
enlarged and swollen. The cartilage, because of
impaired nourishment, lose their elasticity and Income
dry and brittle. The secretion of the synovial membrane
may also diminish and with the progress of the disease,
may cease completely. The joint will thus dry out,
become congested. rough and stir)‘. This may also cause
the surrounding ligaments and tendons to become
inflamed and to progressively lose their tone and flexibility.
Because of the impaired metabolism and movement,
excessive amounts of calcium and other minerals are
deposited in the joints. Sometimes osteoporosis or
leaching of the calcium and other minerals from the
bones can cause severe destruction of bones and joints.
All these changes are usually accompanied with-
swelling and pain during movement. Subsequently, the
pain becomes absolutely incapable of moving the affected
part of the body. If this development is not checked and
eflectively treated in time, complete destruction of the
joint and impairment of its function will often be the
ultimate result. Along with these signs and symptoms in
the joint, the patient also suffers from other disabilities
in difierent parts of the body. Digestive disorders, often
very chronic, are present in patients of arthritis.
Constipation is often prevalent for many years before the
actual arthritis symptoms begin to reveal themselves.
General fatigue, physical and emotional stress, lack of
sufficient rest, nutritional deficiencies, glandular dis-
orders—all these could occur long before the final
symptoms appear in the joints.
It is important therefore to note that if arthritis is to
be successfully treated, the physician should follow a
holistic approach by recognizing the systemic nature of
the disease and the abnormal conditions as well as
disorders in other parts of the body that need to be
corrected. The present-day approach to the treatment of
arthritis patients, namely, to suppress the pain to give
relief to the inflammation or swelling, does only give a
false sense of relief to the patient; it is dangerous because
the disease continues to progress inside the body and at
one stage or the other, both the patient and the
physician become helpless-the former cannot work with
his joints and the latter cannot reduce the pain and
swelling not to speak of arresting the progress of the
disease. Any attempt, therefore, to treat the patient of
arthritis without realising the close relationship between
the general health of the individual and his arthritis
symptoms will ultimately prove to be futile. Joints in
any part of the body maybe aflected. Depending upon
the nature of the affliction. the disease is called by
different names.
The mechanical construction of our body makes it
possible for many bones to meet with each other and
these meeting places are called joints. These joints help
in different types of movements. To avoid friction and
strain during these movements, the ends of the bone are
covered with an elastic tissue called cartilage. A synovial
membrane covers the inner surfaces of this joint-
cavities. This membrane secretes a fluid that lubricates
the joint.
This synovial membrane and the tips of the bones are
ramified with several capillaries which carry. nourishment
along with blood to the joints. If any infection or wrong
metabolic byproduct passes through these capillaries,
then the circulation of the nutrients and blood is
obstructed resulting in stagnation and exudation of fluid
into the pocket created by the synovial membrane in the
joint. This causes the joints to become inflamed,
enlarged and swollen. The cartilage, because of
impaired nourishment, lose their elasticity and Income
dry and brittle. The secretion of the synovial membrane
may also diminish and with the progress of the disease,
may cease completely. The joint will thus dry out,
become congested. rough and stir)‘. This may also cause
the surrounding ligaments and tendons to become
inflamed and to progressively lose their tone and flexibility.
Because of the impaired metabolism and movement,
excessive amounts of calcium and other minerals are
deposited in the joints. Sometimes osteoporosis or
leaching of the calcium and other minerals from the
bones can cause severe destruction of bones and joints.
All these changes are usually accompanied with-
swelling and pain during movement. Subsequently, the
pain becomes absolutely incapable of moving the affected
part of the body. If this development is not checked and
eflectively treated in time, complete destruction of the
joint and impairment of its function will often be the
ultimate result. Along with these signs and symptoms in
the joint, the patient also suffers from other disabilities
in difierent parts of the body. Digestive disorders, often
very chronic, are present in patients of arthritis.
Constipation is often prevalent for many years before the
actual arthritis symptoms begin to reveal themselves.
General fatigue, physical and emotional stress, lack of
sufficient rest, nutritional deficiencies, glandular dis-
orders—all these could occur long before the final
symptoms appear in the joints.
It is important therefore to note that if arthritis is to
be successfully treated, the physician should follow a
holistic approach by recognizing the systemic nature of
the disease and the abnormal conditions as well as
disorders in other parts of the body that need to be
corrected. The present-day approach to the treatment of
arthritis patients, namely, to suppress the pain to give
relief to the inflammation or swelling, does only give a
false sense of relief to the patient; it is dangerous because
the disease continues to progress inside the body and at
one stage or the other, both the patient and the
physician become helpless-the former cannot work with
his joints and the latter cannot reduce the pain and
swelling not to speak of arresting the progress of the
disease. Any attempt, therefore, to treat the patient of
arthritis without realising the close relationship between
the general health of the individual and his arthritis
symptoms will ultimately prove to be futile. Joints in
any part of the body maybe aflected. Depending upon
the nature of the affliction. the disease is called by
different names.